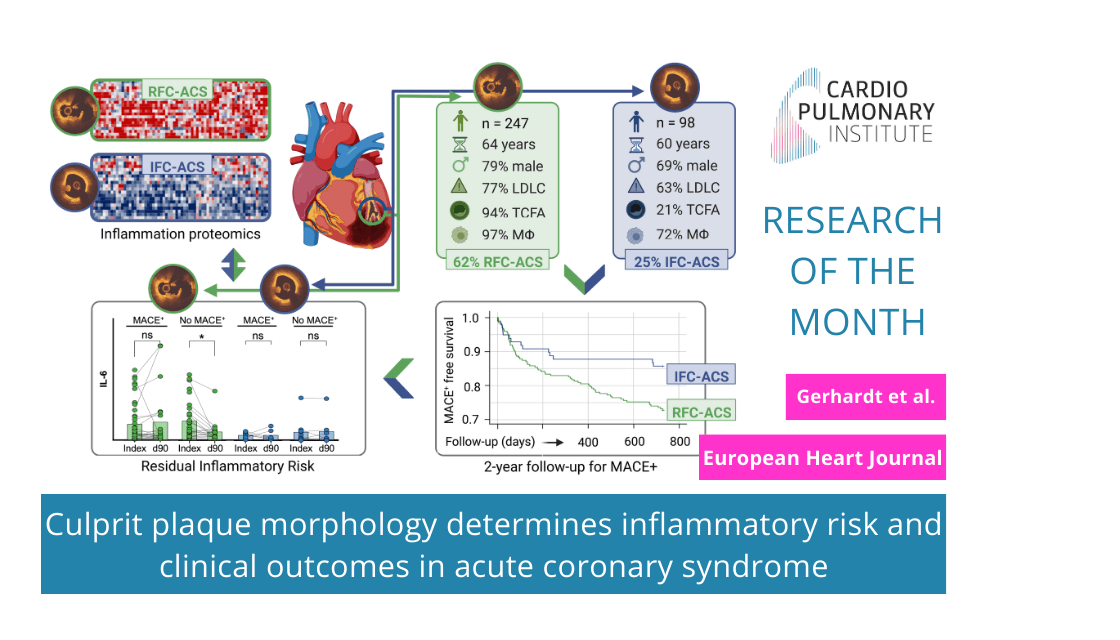
Within recent years the tremendous importance of inflammation in the genesis and aggravation of coronary atherosclerosis ultimately leading to acute coronary syndrome (ACS) has become more and more evident. Recently the CANTOS- and COLCOT-Trials showed anti-inflammatory therapy as a potential secondary prophylactic therapeutic approach. This therapeutic strategy however, resulted in potentially serious side effects such as severe infections, so that a specification of the population benefiting from such therapies became necessary. For this the OPTICO-ACS study aimed to further characterize different ACS causing pathophysiologies with regard to their clinical prognosis and their residual inflammatory risk (RIR), in a prospective, translational approach. It could be shown that patients suffering from a “plaque rupture” (RFC-ACS) had a significantly worse MACE+ free survival rate over 2 years than patients with a “plaque erosion” (IFC-ACS). Furthermore, RFC-ACS patients suffering from a MACE+ defined event had higher levels of inflammation as measured by a 368-plex proteomic analyses and higher levels of IL-6 and hsCRP at index that remained elevated 3 months after inclusion, symbolizing a significant remaining inflammatory risk (RIR). On the other hand, this effect was not seen in RFC-ACS- patients without MACE+ event or IFC-ACS patients.
These findings advance our understanding of inflammatory cascades associated with different mechanisms of plaque disruption and provide hypothesis-generating data for personalized anti-inflammatory therapeutic allocation to ACS patients, a strategy that merits evaluation in future clinical trials.
Find the full article here: